- Mail us: support@drtimpearce.com
The Hidden Risk of Parallel Injections
You may be interested
 Dr Tim Pearce
Dr Tim Pearce
And How to Avoid Them
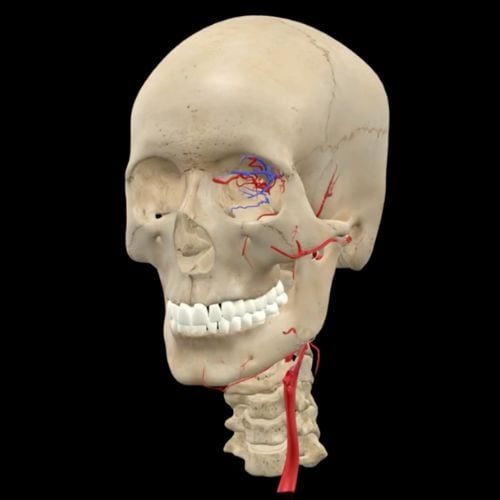
You’ve been taught to avoid blood vessels. You know the names of the big arteries and probably learned where they are on a diagram. But what many injectors don’t realise is that one of the most dangerous techniques isn’t about location – it’s about angle.
Injecting parallel to an artery dramatically increases your risk. Unlike perpendicular injections where your needle might bounce off a vessel or simply pass across it, a parallel injection can slide alongside the artery, making it much easier to cannulate the vessel without resistance. This increases the likelihood of filler being delivered directly into the bloodstream—an event that could lead to complications like occlusion, necrosis, or even blindness.
Let’s explore how this risk shows up in clinical practice and the subtle ways to shift your technique to stay safe.
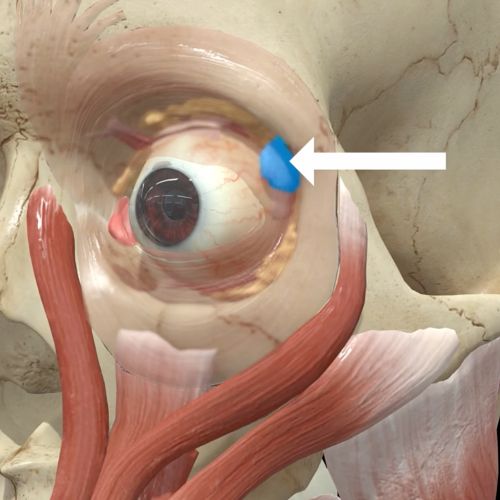
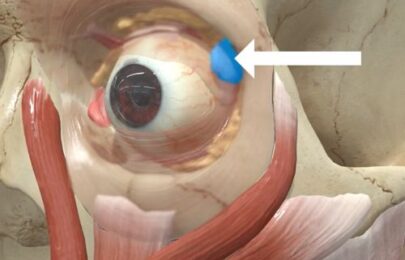
One of the most at-risk areas is the nose, particularly along the dorsum. The dorsal nasal arteries run just lateral to the midline and are aligned in such a way that the common cannula entry points many injectors use put them nearly parallel to the artery’s path. This means that a seemingly routine pass with a cannula could unknowingly place the tip inside the artery. If filler is then injected, it can track upward toward the ophthalmic artery, raising the risk of vision loss. To avoid this, many clinicians choose periosteal needle injections in this region or ensure that they are constantly moving the cannula, aspirating, and applying vessel compression to reduce the chance of intravascular injection.
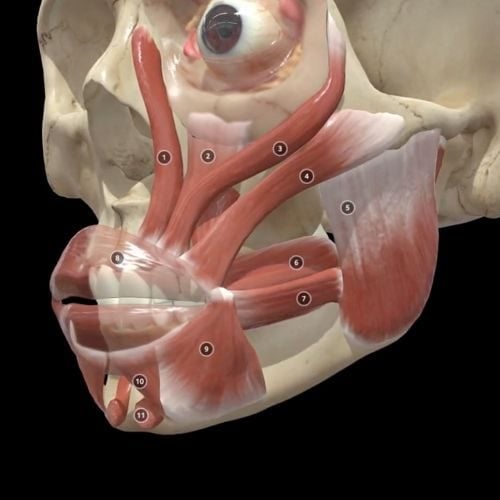
 A similar risk exists in the nasolabial fold. The facial artery courses beneath this area and then turns upward toward the side of the nose. Injectors often thread a cannula through the nasolabial fold from a lateral entry point—an approach that runs nearly parallel to the artery. While deep injections are sometimes seen as safer due to the artery’s more superficial location, poor technique or aggressive passes can still result in intravascular placement. Staying deep and on bone with controlled needle injections has been shown to reduce this risk.
A similar risk exists in the nasolabial fold. The facial artery courses beneath this area and then turns upward toward the side of the nose. Injectors often thread a cannula through the nasolabial fold from a lateral entry point—an approach that runs nearly parallel to the artery. While deep injections are sometimes seen as safer due to the artery’s more superficial location, poor technique or aggressive passes can still result in intravascular placement. Staying deep and on bone with controlled needle injections has been shown to reduce this risk.
Another high-risk zone is the lips. The labial arteries lie just beneath the orbicularis oris muscle, running along the curve of the lip itself. When injectors place product too deep—especially with a linear threading technique—they risk entering this vessel lengthwise. The depth accuracy here is everything. Experienced injectors work with millimeter precision, often using visual cues and tactile feedback to verify they are in the right plane. New injectors often lack this resolution, and being just 2–3mm too deep can lead to intravascular placement. A simple technique to mitigate this risk is aspirating before every injection and ensuring the full outline of the needle or cannula is visible beneath the tissue.
One lesser-known but increasingly popular injection is for lifting the nasal tip. Some techniques involve injecting down the columella to lift the tip upward, but this can position the injector in a line parallel to the columellar artery. The danger here is not just the depth but the volume. A single high-volume injection along this plane increases the risk of occlusion. It’s safer to break the injection into smaller, distributed passes, staying mindful of the anatomical layers beneath.
In the forehead, the supratrochlear artery presents a unique challenge. It lies superficially just beneath the glabellar skin, and often runs parallel to injections intended to fill deep frown lines. Many fillers are contraindicated in this region due to the potential for pressure-related complications. Even with soft fillers, high pressure or excessive volume in this tight space can disrupt capillary flow and cause skin necrosis. Blocking the supratrochlear foramen with manual compression during injection is one added safety measure, as is aspirating and confirming superficial depth visually.
While arteries tend to get all the attention, there’s another risk that arises from parallel injection paths: capillary compression. This isn’t about entering a vessel—it’s about squashing them with filler. Areas like the tip of the nose, the chin, and the glabella are high-risk zones for this type of complication. The dermis in these areas is often thick and immobile, and if you inject a dense product under pressure, the filler can physically compress the microvasculature. The result is a form of ischemia similar to a pressure sore. The best way to avoid this is to test the tissue’s flexibility beforehand. If the skin doesn’t lift easily when pinched, proceed with caution or choose a different approach entirely.
To inject safely, injectors must stack multiple safety practices. Depth awareness is crucial—knowing not just the general anatomy, but the likely depth of each vessel based on the patient’s age, gender, and facial structure. Aspiration should be routine, but not relied upon as a sole safeguard. Manual compression, use of soft products in risky areas, low injection volumes, and ongoing motion with cannulas are all small habits that compound to improve patient safety.
The biggest difference between novice and expert injectors often comes down to “resolution.” Not visual resolution, but anatomical resolution—the ability to see, in your mind, the precise layers of the face and where your needle tip is in relation to key structures. This resolution is what helps you adjust in real time and avoid the kind of parallel injection paths that lead to complications.
If you’d like to learn the safer, smarter way to inject, join Dr Tim for his free live webinar on clinical anatomy for injectors. In this session, you’ll explore high-risk zones in detail, learn how to choose injection angles that avoid arterial paths, and refine your depth perception for safer treatment outcomes.
👉 Reserve your seat for Dr Tim’s next anatomy webinar here.
Protect your patients—and your peace of mind—by mastering the anatomy that matters most.
Related Articles
 Bestseller
Bestseller
Avoiding Botox Eye Complications From Dry Eye to the ‘Psycho Look’
September 30, 2025
Avoiding Botox Eye Complications From Dry Eye to the ‘Psycho Look’
 Bestseller
Bestseller
How to Fix a Crooked Smile with Botox
September 25, 2025
How to Fix a Crooked Smile with Botox
 Bestseller
Bestseller
Multiple Causes of Vascular Occlusion and Necrosis
September 23, 2025